Power Wheelchair Prescription
The following guidelines are based on Medicare. Many private insurances base their requirements on Medicare guidelines so the information provided here will give you a general idea of what to expect. Medicaid coverage varies by state. It is best to work with your local vendor Assistive Technology Professional (ATP) who usually has experience with specific private insurances and Medicaid. If you have Veterans Administration (VA) benefits, you would be best served to discuss this with your medical team at the VA.
- What kind of power wheelchair (PWC) do I need?
- Do I qualify for a power wheelchair?
- Why would I want a group 3 power wheelchair vs group 2 power wheelchair?
- How do I qualify for a group 3 power wheelchair?
- What are the available power seating options and how do I qualify for them?
- What are the roles and responsibilities of the parties involved in the evaluation, prescription and provision of the wheelchair?
- How do I start the process of obtaining a wheelchair?
- What documentation is needed?
- Where can I find examples or get help writing my Letter of Medical Necessity?
- When can I get a new wheelchair?
- What are some considerations to think about prior to getting my wheelchair?
What kind of power wheelchair (PWC) do I need?

Weight capacities: Heavy Duty PWC is covered for a beneficiary weighing 285 – 450 pounds; a Very Heavy Duty PWC is covered for a beneficiary weighing 428 – 600 pounds; an Extra Heavy Duty PWC is covered for a beneficiary weighing 570 pounds or more
Power Wheelchair Bases include the following components:
Lap belt or safety belt, battery charger, tires and casters, leg rests, footrests, armrests, any weight specific components (braces, bars, upholstery, brackets, motors, gears, etc.) as required by beneficiary weight capacity, controller and input device.
For additional information on power wheelchair bases see Local Coverage Article: Power Mobility Devices - Policy Article (A52498)
https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleId=52498
Do I qualify for a power wheelchair?
- I have a mobility limitation that significantly impairs my ability to participate in mobility-related activities of daily living (MRADLs) such as toileting, feeding, dressing, grooming, and bathing in customary locations in the home.
- The mobility limitation cannot be sufficiently resolved with a cane or walker.
- I cannot safely and efficiently self-propel a manual wheelchair.
- I am unable to safely transfer, operate the tiller steering system, and maintain postural stability and position of scooter
- I have appropriate judgement and physical capabilities for safe mobility
- My weight is less than 95% of the max capacity of the wheelchair.
- Use of the power wheelchair will significantly improve my ability to participate in MRADLs and will be used on a regular basis in the home.
- I have not expressed an unwillingness to use the power wheelchair.
- I will have a specialty evaluation that was performed by a licensed/certified medical professional (LCMP) such as a PT or OT, or physician who has specific training and experience in rehabilitation wheelchair evaluations and documentation of medical necessity for the wheelchair and its special features.
- The wheelchair will be provided by a Rehabilitative Technology Supplier (RTS) that employs a RESNA-certified Assistive Technology Professional (ATP) who specializes in wheelchairs and who has direct, in-person involvement in the wheelchair selection for the user.
Why would I want a group 3 power wheelchair vs group 2 power wheelchair?
A group 3 has the following attributes:
- Longer battery life to last all day.
- Faster speed to improve community access.
- Able to get over 2.5” threshold (as opposed to 1.5” required for grp 2)
- Improved suspension to reduce chances of tipping on uneven terrain, smoother ride to reduce spasms, improved ability to navigate thresholds, curbs, and other obstacles.
- Alternative specialty drive controls.
- Multiple drive profiles to optimize performance to multiple environments.
How do I qualify for a group 3 power wheelchair?
Specific Coverage Eligibility:
Group 3 Power Wheelchair (PWC)
- A Group 3 PWC with no power seating options is covered if:
- My mobility limitation is due to a neurological condition, myopathy, or congenital skeletal deformity
- A Group 3 PWC with single or multiple power seating options is covered if:
- My mobility limitation is due to a neurological condition, myopathy, or congenital skeletal deformity; and
- I require a drive control interface other than a hand or chin-operated standard proportional joystick (examples include but are not limited to head control, sip and puff, switch control) OR
- I meet coverage criteria for a power tilt or a power recline seating system (see Wheelchair Options and Accessories policy for coverage criteria) and the system is being used on the wheelchair OR
- I use a ventilator which is mounted on the wheelchair.
- My mobility limitation is due to a neurological condition, myopathy, or congenital skeletal deformity; and
What are the available power seating options and how do I qualify for them?
Power Seating Options
- Tilt and/or Recline
-
- I am at high risk for development of a pressure ulcer and am unable to perform a functional weight shift; or
- I independently utilize intermittent catheterization for bladder management and am unable to independently transfer from the wheelchair to bed; or
- The power seating system is needed to manage increased tone or spasticity.
- Elevating Legs
- I have a musculoskeletal condition or the presence of a cast or brace which prevents 90 degree flexion at the knee; or
- I have significant edema of the lower extremities that requires an elevating leg rest; or
- I meet the criteria for and has a reclining back on the wheelchair.
- Power Adjustable Seat Height
- I perform weight-bearing transfers to/from my power wheelchair while in my home, using either my upper extremities during an uneven sitting transfer or my lower extremities during a sit to stand. This can be performed with or without caregiver assistance and/or use of assistive equipment (e.g. sliding board, cane, crutch, walker, etc)
- I perform a dependent transfer to/from my power wheelchair within the home. This may be accomplished with or without a floor or mounted lift.
- I perform reaching from the power wheelchair to complete one or more mobility-related activity of daily living which may include toileting, feeding, dressing, grooming, and bathing. This can be accomplished with or without caregiver assistance and/or use of assistive equipment.
- Power Standing
- Not a covered benefit under Medicare. Consider alternative funding sources such as vocational rehab, private pay, or grant funding
For additional coverage criteria see Local Coverage Determination (LCD): Power Mobility Devices (L33789)
https://www.cms.gov/medicare-coverage-database/view/lcd.aspx?lcdid=33789&ver=35&
For additional information on Wheelchair Options/Accessories see Local Coverage Determination (LCD): Wheelchair Options/Accessories
What are the roles and responsibilities of the parties involved in the evaluation, prescription and provision of the wheelchair? 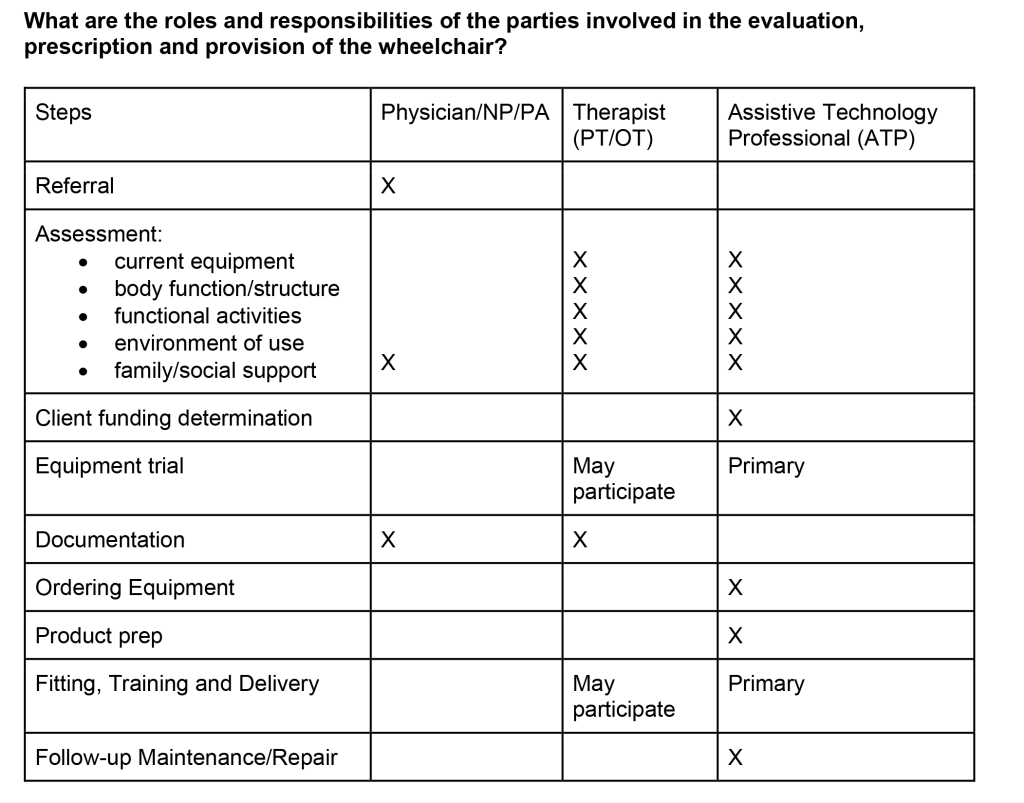
Table developed from RESNA Wheelchair Service Provision Guide https://www.resna.org/Portals/0/Documents/Position%20Papers/RESNAWheelchairServiceProvisionGuide.pdf
How do I start the process of obtaining a wheelchair?
- You will need to work with a prescriber, a PT/OT specialized in wheelchair evaluation, and a vendor ATP. Contact your prescriber for a referral to a therapist and vendor ATP.
What documentation is needed?
- Required documentation includes face to face evaluation by a prescriber, medical record information, Letter of Medical Necessity (typically written by the prescribing therapist in consultation with vendor ATP and signed by the prescriber), and Standard Written Order (SWO).
- The vendor ATP will also need to provide Correct Coding and Proof of Delivery.
Where can I find examples or get help writing my Letter of Medical Necessity?
- Many wheelchair manufacturers have sample letters and offer suggestions for justifying their equipment on their websites.
- Vendor ATP can be a helpful resource for what requires separate justification.
- Consider using standardized forms (searchable online) such as “Houston Methodist Functional Mobility and Wheelchair Assessment” or “Wheeled Mobility and Seating Evaluation”
When can I get a new wheelchair?
- Cannot be a current inpatient at a hospital or skilled nursing facility when you take possession of a new wheelchair.
- Contact your vendor to determine if your existing wheelchair is repairable or modifiable to meet your existing needs.
- If you do not know the vendor, look for a sticker with contact information on the wheelchair frame.
- The wheelchair may require replacement if:
- The current wheelchair /DME is irreparable or determined to be cost-prohibitive to repair or modify in lieu of replacement.
AND/OR - There is a significant and documented change in the patient's medical condition. A new wheelchair may be prescribed to prevent further medical complications or deterioration, e.g., significant weight gain/loss, functional status change (need for PWC and currently has MWC or vice versa), pressure sores, orthopedic issues, aging issues, etc. Clear documentation as to why the current mobility device cannot be modified to accommodate these changes should be included in the equipment justification statement.
- The current wheelchair /DME is irreparable or determined to be cost-prohibitive to repair or modify in lieu of replacement.
What are some considerations to think about prior to getting my wheelchair?
- Will it fit in my home?
- A home evaluation is required prior to ordering a wheelchair. This is done by your vendor ATP.
- Home evaluation includes ramp entry to/from outdoors, adequate doorway widths including bathroom, bedroom, kitchen
- Talk to your vendor ATP to estimate final wheelchair width.
- How will I transport the chair outside of my home?
- Will it fit in my vehicle?
- Does my lift have sufficient weight capacity?
- Does my vehicle have sufficient head clearance if I am staying in the chair during transportation?
- Will I be able to do the activities I love to do?
- You should try the new equipment and discuss concerns with your vendor and/or therapist before ordering to ensure it meets your needs.
Authorship
- Resource Sheet on Power Wheelchair under Medicare Guidelines was developed by Tara Businski, PT, DPT, ATP, Margaret Dahlin, PT, DPT, ATP, Michelle Graf, OTR/L, and as well as the CRT subcommittee of the ASCIP Advocacy Committee.
Disclaimer
- This information is intended for rehabilitation professionals and may be shared with consumers with SCI/D. This resource sheet is not meant to replace the advice from a medical / rehabilitation professional. Medical / rehabilitation professionals are encouraged to discuss this material with consumers in the context of their overall medical rehabilitation care.